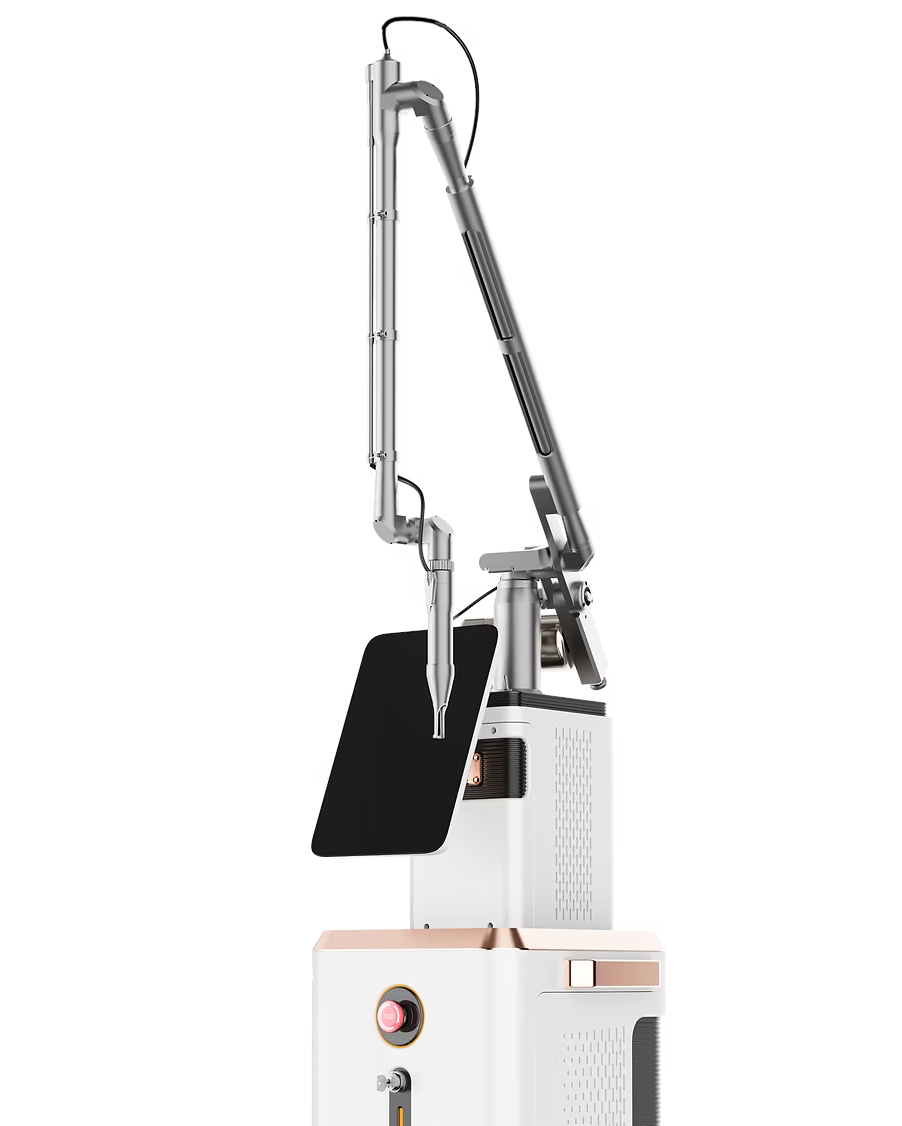
Periodontal
Laser Assisted Periodontal Therapy
A Minimally Invasive Solution for Healthier Periodontal Outcomes
Laser assisted periodontal therapy provides a minimally invasive approach that supports cleaner, more predictable treatment outcomes. The controlled penetration depth of the CO₂ 10,600 nm wavelength allows clinicians to selectively remove diseased epithelium while simultaneously disinfecting the sulcus. This dual action helps reduce bacterial load, encourage healthier tissue response and support natural metabolic healing processes, often without the need for traditional flap surgery. The result is a patient friendly method that promotes comfort, efficiency and long term periodontal stability.
Limiting the Iatrogenic Nature of Traditional Procedures
Traditional mechanical instruments, while effective, also pose the risk of unintentionally transferring bacteria to healthy tissue. CO₂ laser technology minimizes this risk by disinfecting as it selectively vaporizes diseased epithelium. Using the laser as an adjunct to conventional periodontal therapy helps create a cleaner environment for regeneration and reduces the potential for postoperative inflammation. The key advantages are:
Reduced risk of bacterial transfer
Selective removal of diseased epithelium
Cleaner periodontal environment
Enhanced tissue preservation
Improved clinical predictability
Therapy Supported by Evidence Based Research
Decades of scientific research support the effectiveness of laser assisted periodontal therapy as an adjunct to traditional periodontal treatment. The CO₂ wavelength enhances tissue response by reducing bacterial activity, limiting inflammation and supporting healthier attachment.
The minimally invasive nature of this approach allows clinicians to provide more comfortable procedures with reduced bleeding and improved postoperative outcomes.
Understanding Laser Assisted Periodontal Therapy
Laser assisted periodontal therapy functions as a supportive tool rather than a standalone treatment. Foundational periodontal principles such as scaling, root planing, mobility assessment and occlusal evaluation remain essential. However, incorporating laser technology significantly enhances the healing environment by reducing bacterial load and limiting epithelial invasion. The CO₂ wavelength can de epithelialize the pocket lining without the need to raise a flap, allowing for selective tissue removal and improved regenerative potential. This creates favorable conditions for tissue repair and decreases pocket depth without relying on long junctional epithelium.
Deepithelialization: A Transformative Advancement
A unique feature of the super pulsed 10,600 nm CO₂ wavelength is its ability to selectively dehydrate and remove crestal epithelium. By delaying apical epithelial migration, the laser helps prevent rapid downgrowth that would otherwise limit regenerative potential. This extended healing window allows the body more time to regenerate bone and cementum, creating an environment that supports healthier long term periodontal outcomes. The regenerative advantages are:
Delayed epithelial migration
Improved regenerative potential
Enhanced bone and tissue healing
Support for long term periodontal stability